Cervical cancer vaccine or HPV vaccine
Most cervical cancers are linked to the human papillomavirus (HPV), a sexually transmitted disease. Widespread HPV vaccination could reduce the impact of HPV-caused cervical and such other cancers worldwide. HPV vaccines prevent infection by certain types of human papillomavirus. The available HPV vaccines can guard against either two, four, or nine types of HPV. All HPV vaccines guard against minimum HPV types 16 and 18, which is responsible for the greatest risk of cervical cancer.
What is cervical cancer?
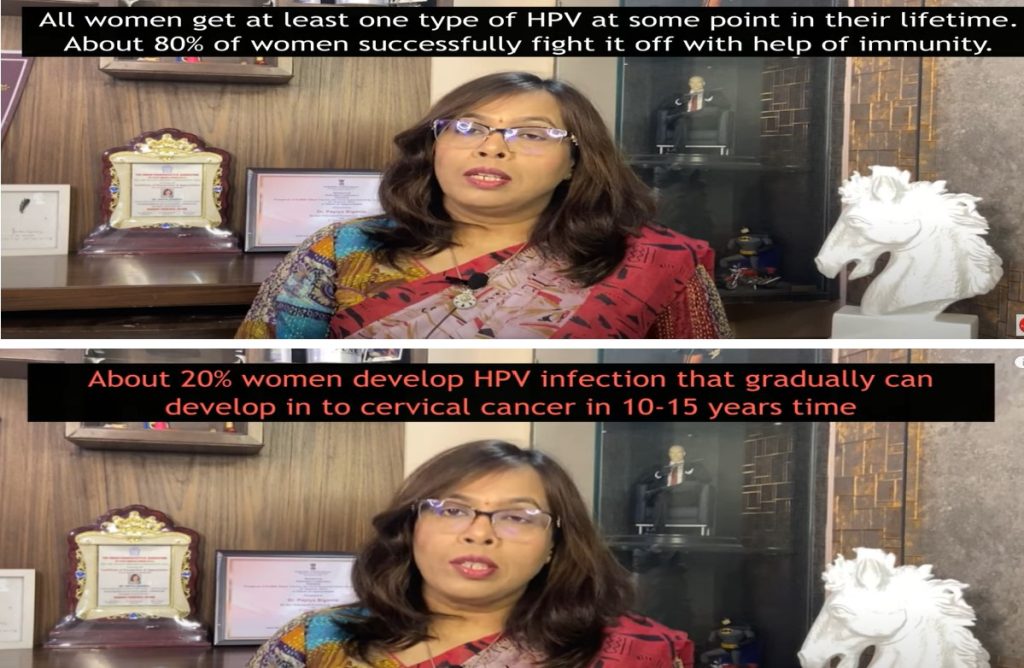
Cervical cancer occurs in the cervix, the lower, narrow end of the uterus (womb). Cervical cancer usually develops slowly over time. Human papillomavirus is a very common group of viruses causing genital warts or cancer. Human papillomavirus (HPV) usually goes away on its own without any treatment, but in some females, it can cause cervical cancer. HPV is estimated to cause more than 8 lakh cases every year. HPV vaccination can prevent 705 cervical cancer-related deaths.
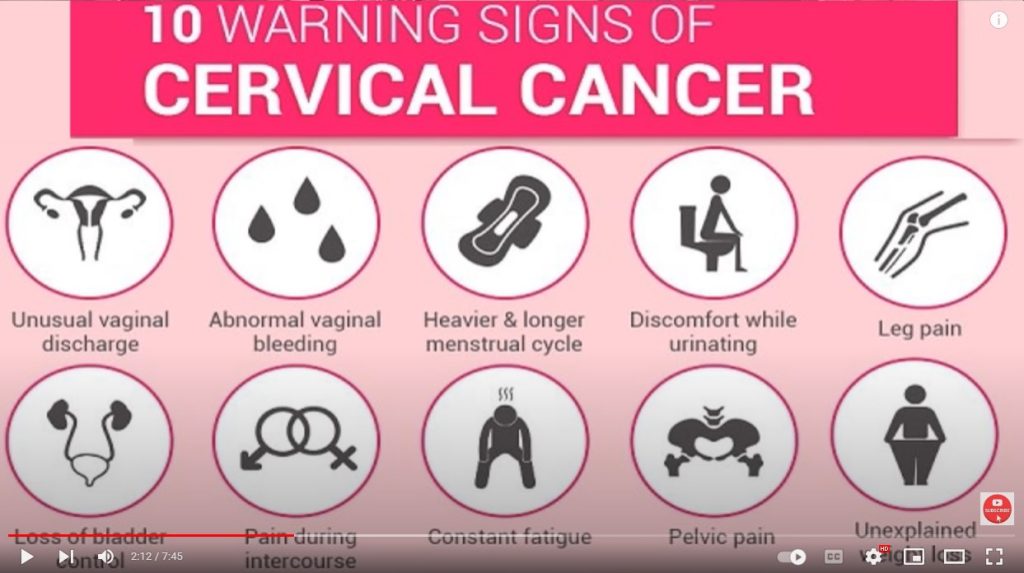
Signs and symptoms of cervical cancer
- Vaginal bleeding after sex or menopause
- Pelvic pain
- Pain during sex
Although these signs and symptoms may be due to other conditions also. To confirm, an opinion from an expert is advisable.
Diagnosis of cervical cancer
It is difficult to diagnose cervical cancer in the early stage. The reason is that as such there are no prominent symptoms of it and it is left unnoticed.
Types of cervical cancer vaccine or HPV vaccine
Three types of HPV vaccines are the 9-valent HPV vaccine (Gardasil 9, 9vHPV), the quadrivalent HPV vaccine (Gardasil, 4vHPV), and the bivalent HPV vaccine (Cervarix, 2vHPV). All three HPV vaccines had one common aspect that it protects against HPV types 16 and 18 that cause most HPV cancers (About 70%). Gardasil-9 (9vHPV) is the vaccine that protects against nine HPV types (6, 11, 16, 18, 31, 33, 45, 52 and 58). According to the Indian Society of Coloscopy and Cervical Pathology, high-risk HPV strains 31, 33, 45, 52, and 58 are responsible for an additional 10% to 20% of cervical cancer cases.
Names of cervical cancer vaccine or HPV vaccine
Various existing marketed cervical cancer vaccines are:
| Name | Type | Effective Against | Manufacturer |
| Gardasil | Quadrivalent | HPV types 6, 11, 16, and 18 | Merck |
| Gardasil 9 | Nonavalent | HPV types 6, 11, 16, 18, 31, 33, 45, 52, and 58 | Merck |
| Cervarix | Bivalent | HPV types 16 and 18 | GlaxoSmithKline |
| Cecolin | Bivalent | HPV types 16 and 18 | Innovax Biotech Co. |
| Walvax | Bivalent (Recombinant) | HPV types 16 and 18 | Watson Bio. |
| CERVAVAC (Made-In-India) First Indian HPV Vaccine from Serum Institute, Pune, India | Quadrivalent | HPV types 6, 11, 16, and 18 | Serum Institute, Pune, India |
Cost of cervical cancer vaccines or HPV vaccine
The average cost of dosing for all international vaccines ranges from INR 3000 to 10000 per dose. Serum Institute of India launched the first made-in-India HPV vaccine for cervical cancer. This indigenously developed vaccine, is called CERVAVAC that will be ready for market circulation by May -June this year (2023). The average cost of two does are expected to be below 500 INR (cost may be even lower in the future).
About CERVAVAC- the First Indian cervical cancer vaccine or human papillomavirus (HPV) vaccine
Facts and figures available about CERVAVAC vaccine are
- The first Indian cervical cancer vaccine or human papillomavirus HPV vaccine (qHPV) was manufactured by the Pune-based Serum Institute of India (SII).
- Approved by The Drugs Controller General of India (DGCI).
- jointly shaped by the SII and the Department of Biotechnology (DBT).
Age for cervical cancer vaccine or HPV vaccine
- Age of Dose 1: 11-12 years or can be started at the age of 9 years
- Age of Dose 2: After 6-12 months of the first dose
Cervical cancer or HPV vaccines are recommended to girls between ages 11 and 14. Though it can be given as early as age 9, but the ideal age for girls for HPV vaccination is before they have sexual contact and are exposed to HPV. HPV vaccinations can be taken between ages 25-45 who are not adequately vaccinated, but the efficacy reduces. Generally HPV haccination is not suitable after the age of 26 years.
Dose of cervical cancer vaccines or HPV vaccine
- 2 Doses: 11-12-year-old children
- 3 Doses: If vaccination starts at ages between 15 to 24
Girls need to receive two doses of the HPV vaccine at least six months apart. Girls at younger adolescents age 15 to 24 need to receive a vaccination on the three-dose schedule. According to CDC, the two-dose schedule of cervical cancer vaccines or human papillomavirus (HPV) vaccines is effective for children under 15 years.
Effectiveness of cervical cancer vaccines or HPV vaccines
According to Research, vaccination with the HPV vaccine at a young age show high efficacy. The efficacy of vaccination with cervical cancer vaccines or human papillomavirus (HPV) vaccines might not be as effective as if it is given after an HPV infection. The effectiveness of the vaccine is better at younger ages than it is at older ages. HPV vaccinations can be taken between ages 25-45 who are not adequately vaccinated, but the efficacy reduces. None of the HPV vaccines can treat an existing HPV infection. The vaccines protect only from specific strains of HPV patients have not been exposed to already.
Cervical cancer vaccines or HPV vaccine in a pregnancy
If a female become pregnant after the first dose should not take the subsequent dose of the HPV vaccine in pregnancy.
Allergic reactions of cervical cancer vaccines or HPV vaccines
For any person or patient or individual who has reported any life-threatening allergic reaction due to any vaccine’s component to a previous dose of the vaccine, vaccination with the HPV vaccine should not be done.
Side effects of HPV vaccines
HPV vaccine is very safe and usually may have some mild side effects that are mild. The most common side effects of these vaccines are
- Soreness
- swelling
- redness at the injection site
- Dizziness or fainting
- Headache
- Nausea
Cervical cancer vaccines or HPV vaccines for male
The U.S. Food and Drug Administration (USFDA) freshly approved the use of Gardasil 9 for males and females ages 9 to 45. In countries like the US, Australia and UK HPV vaccines are recommended for males also as this vaccine is effective against genital warts and cancers of the genital tract. Overall, HPV vaccine is very safe and usually may have some mild side effects that are mild.
Cervical cancer occurs in the cervix, the lower, narrow end of the uterus (womb). Cervical cancer usually develops slowly over time. Human papillomavirus is a very common group of viruses causing genital warts or cancer. Human papillomavirus (HPV) usually goes away on its own without any treatment, but in some females, it can cause cervical cancer. HPV is estimated to cause more than 8 lakh cases every year. HPV vaccination can prevent 705 cervical cancer-related deaths. In this video Dr. Papiya Bigoniya is explaining about causes, symptoms, and severity of cervical cancer, and how vaccines can save many lives.
Mechanism of action of cervical cancer vaccine or HPV vaccine
To learn about the pharmacology and mode of action of the vaccine, please see https://www.youtube.com/watch?v=ggI5bpV4iSI&t=3s. According to the author, cervical cancer can be prevented by the immunization with HPV vaccine.
Conclusion
Cervical cancer is the second largest cancer in women and the cause of death in countries like India. India is a developing country and accordingly, a cost-effective vaccine is need of time for cervical cancer. HPV vaccines available in the current market are very costly and not affordable even to the middle class. CERVAVAC is the first Made in India cervical cancer or HPV vaccine, which has generated real hope to fight against cervical cancer, especially in girls and women. The cost-effectiveness of CERVAVAC will give a new boost to immunization programs in India and other developing and Asian countries against cervical cancer.
Authors: Dr. Papiya Bigoniya, PhD in Pharmacology and Dr. Avijeet Jain, PhD in P’conosy (Pharmaceutical Sciences).
Also Read: What is Biologics and When Does it Matter?


